For anyone who has watched a friend with Type 1 diabetes politely refuse a slice of birthday cake, or has seen a child have to stop playing to prick their finger for the fifth time in a day, the idea of a cure has always felt like a distant, almost impossible dream. It was a hope whispered for “someday,” for a future that never seemed to get closer.
This week, that dream took a giant leap toward reality.
In findings that have sent waves of excitement through the medical community, a new experimental stem-cell therapy is showing stunning success in treating the most severe forms of Type 1 diabetes. In a landmark clinical trial, 10 out of 12 patients who received a single infusion of the treatment, called Zimislecel, are now living completely free from the daily, life-sustaining injections of insulin. A year after their treatment, their own bodies are doing the work that, for decades, they were told was impossible.
For these patients, the result is nothing short of a rebirth. “It’s like a whole new life,” said Amanda Smith, a 36-year-old nurse who participated in the trial. For Illinois mom Marlaina Goedel, who was diagnosed at age five and spent 25 years constantly worrying if she would wake up the next day, the conclusion was even simpler. “I am cured,” she declared. Now, she is chasing long-postponed dreams: riding her horse, going back to school, and soaking in a life no longer dictated by the relentless math of blood sugar numbers.

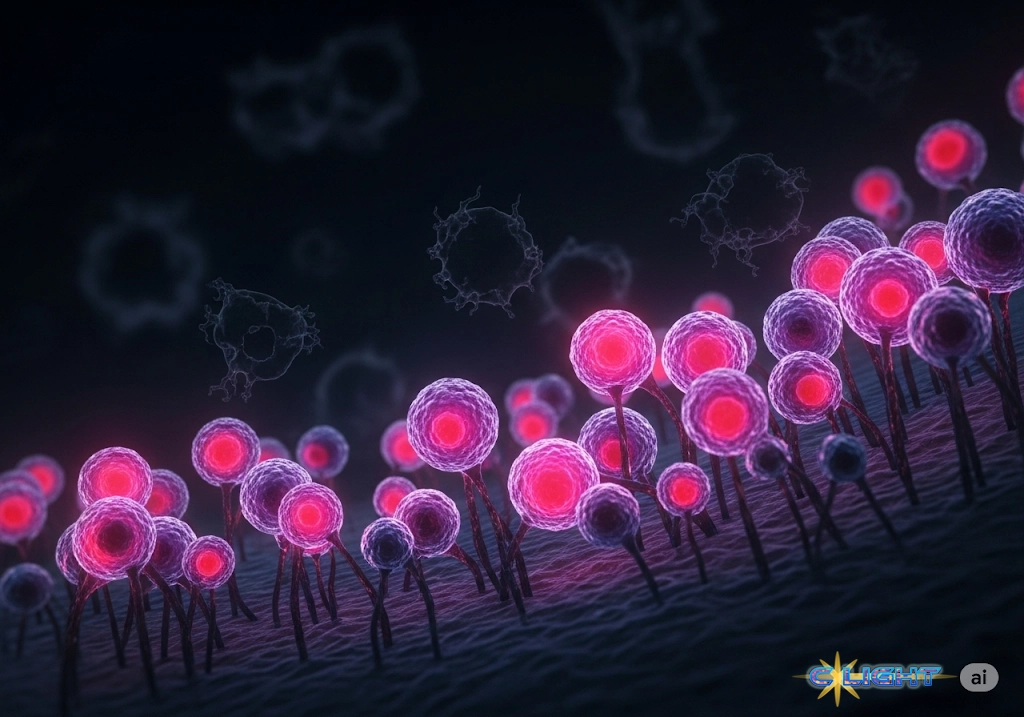
The science behind this breakthrough is as elegant as its results are profound. Developed by Vertex Pharmaceuticals, Zimislecel is not a drug that manages symptoms, but a cell therapy that fixes the underlying problem. Type 1 diabetes is an autoimmune disease where the body’s own immune system destroys the insulin-producing islet cells in the pancreas. This therapy infuses patients with new, healthy islet cells that have been cultivated from stem cells in a lab. These new cells take up residence in the liver and, like a factory coming back online, begin producing the insulin the body needs to function.
Experts are calling it the “holy grail” of diabetes treatment. For decades, doctors have known that transplanting islet cells could work, but the procedure was severely limited by the extreme scarcity of organ donors, often requiring multiple donors for a single patient. This breakthrough provides, in the words of lead study author Dr. Trevor Reichman, an “off-the-shelf, unlimited source of islets,” potentially making a functional cure accessible to the 8.4 million people living with Type 1 diabetes worldwide.
This medical miracle was born from a father’s promise. The research was pioneered over 25 years by Dr. Doug Melton, a brilliant Harvard researcher who dedicated his life to the problem after both his infant son and, later, his teenage daughter were diagnosed with the disease. It was his unwavering belief that science could solve this that laid the foundation for today’s success.
Of course, the road to a universal cure is not yet complete, and the researchers are clear-eyed about the current limitations. As you noted, this therapy is designed for Type 1 diabetes, where the problem is a lack of insulin production; it cannot address the insulin resistance that characterizes the more common Type 2 diabetes.

The other major caveat is the significant trade-off patients must make. To keep their bodies from attacking the newly infused cells, they must take lifelong immunosuppressant drugs, which carry their own serious risks, including a higher susceptibility to infections and cancer. For patients suffering from the most severe complications—like “hypoglycemic unawareness,” where they have no warning of a potentially fatal blood sugar crash—this trade-off is a clear victory. For others, the calculation may be more complex.
But the journey is far from over. The trial has been so successful that it is now advancing to a larger Phase 3 study, a major step on the path to FDA approval. And scientists are already working on the next great challenge. “We hope in the next five to 10 years,” Dr. Reichman said, “that this therapy will have the potential to be given with minimal or zero immunosuppression.”
That is the ultimate goal. But for now, the impossible dream has become a tangible reality. A functional cure for Type 1 diabetes is no longer a question of “if,” but “when.” For millions of families who have measured life in needle pricks and dietary restrictions, hope has a new name.
Discover more from Clight Morning Analysis
Subscribe to get the latest posts sent to your email.